Corneal Transplantation Surgery
Corneal transplantation is also known as corneal grafting. It is a surgical procedure where a damaged or diseased cornea is replaced by donated corneal tissue (the graft) in order to improve or restore vision, preserve/reconstruct corneal anatomy, remove inflamed corneal tissue or to improve corneal scars. It generally takes one to two hours and most procedures are performed on an outpatient basis, meaning you can go home a short while after the surgery. Costs associated with cornea transplant procedures are typically covered by health insurance or Medicare.
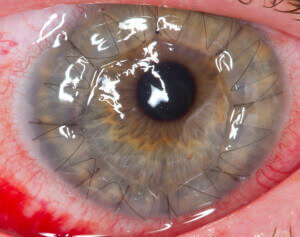
[“A human eye 1 day after a cornea transplant” by Megor1 – Photo taken by me. Licensed under CC BY-SA 3.0 via Wikimedia Commons – https://commons.wikimedia.org/wiki/File:A_human_eye_1_day_after_a_cornea_transplant.jpg]
Penetrating Keratoplasty or Traditional Corneal Transplant – Patients who have corneal disease in the front or throughout the whole cornea are candidates for a traditional corneal transplant, otherwise known as penetrating keratoplasty. Penetrating keratoplasty is preferred when the disease involves irreversible damage.
Lamellar keratoplasty – a corneal transplantation technique that selectively replaces diseased layers of the cornea while leaving healthy layers in place.
Endokeratoplasty – A new corneal transplant technique which enables more selective replacement of the diseased corneal endothelium. This approach is most appropriate for disease processes that exclusively or predominantly involve the corneal endothelium. Compared to traditional corneal transplant, Endokeratoplasty is associated with shorter recovery times, improved visual results, and greater resistance to wound rupture. The most commonly performed forms of endokeratoplasty at present are Descemet’s Membrane Endothelial Keratoplasty (DMEK) and Descemet’s Stripping Automated Endothelial Keratoplasty (DSAEK). In 2009, The American Academy of Ophthalmology endorsed Endokeratoplasty as superior to the traditional cornea transplant for better vision outcomes and stability, as well as fewer risk factors.
According to Eye Bank Association of America, Cornea Transplant performed in the U.S. has a high success rate of 95-99%. And in 2014, 209 corneas were provided for transplant every day.
[Eye Bank Association of America. Home – Eye Bank Association of America [Internet]. 2015 [cited 2015 Jun 1]. Available from: http://restoresight.org/]
Cornea Transplant Risks
Like all surgeries, corneal transplantation does carry with it some risks. They include graft rejection or failure, glaucoma, cataract, and in rare cases, bleeding, infection, or retinal detachment. Many of these complications can be treated with medications or surgery.
Corneal transplantation is an extremely delicate procedure. While vision will start returning several weeks after surgery, months of healing are required before full vision is restored. Glasses, contact lenses, or LASIK may be needed to sharpen vision. Long-term use of eye drops as well as regular office visits are required in order for your transplant to be successful.
Corneal Transplant at Passaic and Bergen Counties, New Jersey

Eye Care Associates of New Jersey has joined the revolution in curing corneal disease. Dr. Adam S. Friend is now performing Descemet’s Stripping Automated Endothelial Keratoplasty (DMEK), a partial thickness corneal transplant that reduces healing time from one year to only several weeks while also being much safer.
In patients who suffer from diseases that affect only the back of the cornea, Dr. Friend can remove the diseased area and leave behind the healthy cornea. He then removes the posterior part of a healthy donor cornea and inserts it into the eye through a small incision. This reduces the risk of sutures rupturing from eye trauma and greatly lessens any astigmatism that can occur from corneal sutures.
We perform corneal transplant surgery at the Bergen-Passaic Cataract Surgery & Laser Center in Glen Rock proudly serving Franklin Lake, Wycoff and surrounding NJ areas.